2023 Public Health Laboratory Annual Report
New Antimicrobial-Resistant Organisms Threaten Public Health
Antimicrobial resistance is recognized as killing at least 1.27 million people worldwide.
 One of the greatest advances in medical science -- the discovery and production of antibiotics to treat and cure people of deadly infectious diseases -- has saved millions of lives worldwide since Alexander Fleming discovered (partially by accident) the antimicrobial properties of penicillin mold in 1928.
One of the greatest advances in medical science -- the discovery and production of antibiotics to treat and cure people of deadly infectious diseases -- has saved millions of lives worldwide since Alexander Fleming discovered (partially by accident) the antimicrobial properties of penicillin mold in 1928.
However, bacteria, viruses, parasites, and fungi are evolving, developing ways to defeat or resist antimicrobial agents like antibiotics. The emergence of antimicrobial-resistant organisms means that infections typically defeated by common antimicrobials have become more difficult to treat, leading to more illnesses and deaths.
The Minnesota Public Health Laboratory has been involved in recent outbreaks of two separate organisms that resist carbapenems, valuable antibiotics that fight bacterial infections. If carbapenem resistance becomes widespread, millions of infections will become much more difficult to treat.
Outbreak One: E. coli in Dogs
In 2022, a dog underwent an operation for a head wound at the University of Minnesota Veterinary Medical Center. A carbapenem-resistant Escherichia coli (E. coli) was found at the site of the wound. The dog lives in a congregate animal rescue facility that supplies therapy animals to assisted living communities.
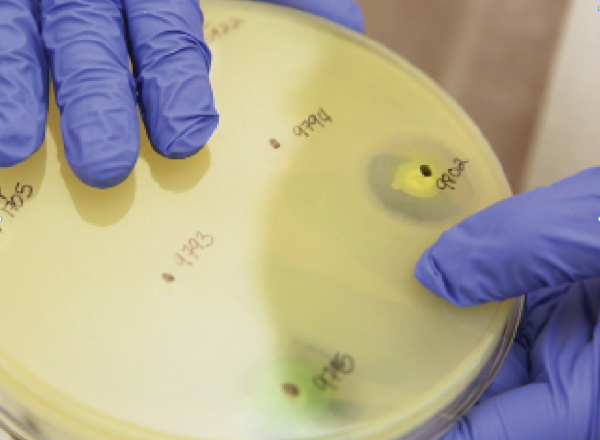
The Infectious Disease Laboratory used its sophisticated instrumentation to determine the gene responsible for carbapenem resistance in the organism: blaNDM. The lab then evaluated samples from 73 dogs from the animal rescue facility and discovered the blaNDM gene in 27 of them. They were colonized by the E. coli, meaning that they carried the organism, but they were not infected, in that they did not have symptoms.
Of the 27 colonized dogs, 20 had been imported from other nations. So far, there have been no documented cases of transmission from animals to humans of the E. coli. Scientists do not yet know how readily the pathogen can spread from dogs to humans.
Outbreak Two: CRPA in Eye Drops
Another antimicrobial-resistant organism has been uncovered across the United States. In October 2022, the CDC discovered an outbreak of carbapenem-resistant Pseudomonas aeruginosa (CRPA). The Minnesota Department of Health sent an alert to labs throughout the state to send any isolates of CRPA to the Public Health Laboratory.
As dozens of CRPA cases were isolated in other states, the CDC investigated each to discover a common source for the organism. A culprit was found: Artificial Tears Lubricant Eye Drops. The product’s manufacturer initiated a voluntary recall after a recommendation by the Food and Drug Administration (FDA).
In mid-March 2023, the Minnesota Public Health Laboratory received an isolate from South Dakota that tested positive for CRPA. The CDC is investigating the case.
On March 21, 2023, the CDC released an update stating that 68 patients in 16 states have been identified as contracting VIM-GES-CRPA. Just four health care facilities, all of which used eye drops from the same manufacturer, are linked to 37 of the patients. Many patients contracted eye infections, eight suffered vision loss, and three died. Since March 21, several more cases have been found, but still none in Minnesota.
By detecting, characterizing, and monitoring such threats quickly after a specimen is discovered, the Minnesota Public Health Laboratory and the rest of the American public health infrastructure gather the information necessary to prevent future epidemics.
The Minnesota Department of Health Public Health Laboratory is one of seven public health laboratories across the nation chosen by the CDC to provide testing in a national surveillance system that monitors and responds to drug resistance throughout the country.
Infectious Disease staff perform highly specialized tests that allow them to respond to outbreaks, characterize and track different mechanisms of resistance, and to detect new kinds of resistance in the pathogens that most concern public health officials.
How Antimicrobial Resistance Happens
Antimicrobial resistance involves bacteria and other pathogens that live in and on our bodies developing the ability to survive the drugs designed to kill them. It does not mean the human body itself is resistant to antibiotics, antifungals, or other medicines.
The pathogens then proliferate further and can even pass on the genes responsible for antimicrobial resistance to other organisms.
- Among many bacteria, a few are drug resistant.
- Antibiotics kill bacteria causing illness, as well as good bacteria protecting the body from infection.
- The drug-resistant bacteria can now grow and take over.
- Some bacteria give their drug resistance to other bacteria.
Return to the main 2023 Annual Report page.