Annual Summary of Disease Activity:
Disease Control Newsletter (DCN)
- DCN Home
- Annual Summary, 2022
- Annual Summary, 2021
- Annual Summary, 2020
- Annual Summary, 2019
- Annual Summary, 2018
- Annual Summary, 2017
- Annual Summary, 2016
- Annual Summary, 2015
- Annual Summary, 2014
- Annual Summary, 2013
- Annual Summary, 2012
- Annual Summary, 2011
- Annual Summary, 2010
- Annual Summary, 2009
- Annual Summary, 2008
- Annual Summary, 2007
- Annual Summary, 2006
- Annual Summary, 2005
- Annual Summary, 2004
- Annual Summary, 2003
- Annual Summary, 2002
- Annual Summary, 2001
- Annual Summary, 2000
- Annual Summary, 1999
- Annual Summary, 1998
- Annual Summary, 1997
Related Topics
Contact Info
Tuberculosis, 2015
In 2015, 150 tuberculosis (TB) cases (2.7 per 100,000 population) were reported. This represents a 2% increase in the number of cases compared to 2014 (147), but a 37% decrease in the number of cases since 2007, when the highest number (238) in the past decade was reported. As seen in most years, Minnesota’s TB incidence rate in 2015 was lower than the national rate of 3.0 cases per 100,000 population. Two (1%) of the cases died due to TB-related causes.
Twenty-three (26%) of the state’s 87 counties reported at least 1 new case of TB disease in 2015. The majority (74%) of cases occurred in the metropolitan area, primarily in Hennepin (38%) and Ramsey (19%) Counties. Seventeen percent (25) were from the other five metropolitan counties. The remaining 26% of cases were reported from Greater Minnesota. Among metropolitan area counties, the highest TB incidence rate in 2015 was reported in Ramsey County (5.4 per 100,000 population), followed by Hennepin County (4.7 per 100,000), and Dakota County (2.7 per 100,000 population). The TB incidence rate for all Greater Minnesota counties combined was 1.6 per 100,000 population.
The vast majority (87%) of TB cases reported in Minnesota in 2015 were identified as a result of individuals seeking medical care for symptoms of disease. Various targeted public health interventions identified a portion of the remaining 13% of cases. Such methods of case identification are considered high priority, core TB prevention and control activities; they included TB contact investigations (3%), follow-up evaluations resulting from abnormal findings on pre-immigration exams performed overseas (3%), and domestic refugee health assessments (2%). An additional 3% were identified through other means (e.g., other immigration medical exams, occupational screening or other targeted testing for TB). Five (3%) cases were diagnosed with active TB disease incidentally while being evaluated for another medical condition.
TB incidence is disproportionately high in racial minorities in Minnesota as well as in the United States. In 2015, only 12 cases occurred among non- Hispanic whites in Minnesota (0.3 cases per 100,000 population). In contrast, among non-Hispanic persons of other races, 84 cases occurred among blacks (24.5 cases per 100,000), 41 among Asian/Pacific Islanders (15.3 cases per 100,000), and 4 among American Indian/Alaskan Natives (6.0 cases per 100,000). Nine cases were Hispanic persons of any race (3.2 cases per 100,000). The vast majority of black TB cases (92%) and Asian TB cases (98%) were foreign-born.
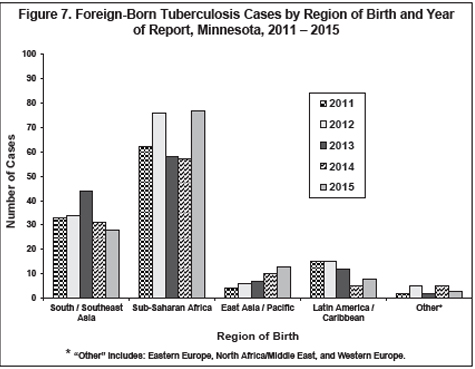
The most distinguishing characteristic of the epidemiology of TB disease in Minnesota continues to be the large proportion of cases occurring among persons born outside the United States. In 2015, the percentage of TB cases in Minnesota occurring in foreign-born persons was 86%, compared to 66% of TB cases reported nationally. The 129 foreign-born TB cases reported in Minnesota represented 26 different countries of birth; the most common region of birth among these patients was Sub-Saharan Africa (60% of foreign-born cases), followed by South/ Southeast Asia (22%), East Asia/Pacific (10%), and Latin America (including the Caribbean) (6%) (Figure 7). All 6 U.S.- born pediatric TB cases (<15 years of age at diagnosis) had at least one foreign-born parent or guardian. These second-generation children appear to experience an increased risk of TB disease that more closely resembles that of foreign-born persons.
Among the foreign-born TB cases, 19% were diagnosed with TB within the first 12 months after arriving in the United States, and an additional 12% were diagnosed 1 - 2 years after arrival. These cases most likely acquired TB infection prior to immigrating and started progressing to active TB disease shortly after arrival. Of the 16 cases ≥15 years of age who arrived as immigrants or refugees and diagnosed in Minnesota within 12 months of arriving in the U.S., only 4 had any TB-related condition noted in their pre-immigration medical examination reports. These findings highlight the need for clinicians to have a high index of suspicion for TB among newly arrived foreign-born persons, regardless of the results of medical exams performed overseas.
Fifty-three percent of cases had pulmonary disease exclusively. Another 11% had both pulmonary and extrapulmonary sites of disease. An equal percentage of foreign-born and U.S.-born TB cases (47%) had at least 1 extrapulmonary site of disease, although extrapulmonary disease is usually more common among foreign-born cases. Among cases with an extrapulmonary site of disease, the most common sites were lymphatic (55%) followed by musculoskeletal (21%).
Aside from foreign-born persons, individuals in other high risk groups comprise a smaller proportion of the TB cases in Minnesota. Twenty-five percent occurred among persons with certain medical conditions (excluding HIV infection) that increase the risk for progression from latent TB infection (LTBI) to active TB disease (e.g., diabetes, prolonged corticosteroid or other immunosuppressive therapy, and end-stage renal disease). Following the presence of these underlying medical conditions, the next most common risk factor was substance abuse (including alcohol abuse and/or injection and non-injection drug use), with 7% having a history of substance abuse during the 12 months prior to their TB diagnosis. Nine (6%) were co-infected with HIV. Three percent reported being homeless during the 12 months prior to diagnosis. Another high risk group accounting for 2% of cases included correctional facility residents at time of diagnosis.
In 2015, of 115 culture-confirmed TB cases with drug susceptibility results available, 16 (14%) were resistant to at least 1 first-line anti-TB drug [i.e., isoniazid (INH), rifampin, pyrazinamide, or ethambutol], including 9 (8%) cases resistant to INH. There were no cases of multidrug-resistant TB (MDR-TB, or resistance to at least INH and rifampin) reported in 2015. In comparison, 24% of culture-confirmed cases in 2014 with susceptibility results available were resistant to at least one first-line anti-TB drug, 18% were resistant to INH, and 1 case had MDR-TB.
- For up to date information see>> Tuberculosis (TB)
- Full issue>> Annual Summary of Communicable Diseases Reported to the Minnesota Department of Health, 2015