Healthcare-Associated Infections
- Healthcare-Associated Infections Home
- About HAIs
- HAIs and Antibiotic Resistance
- Resources
- Drug Diversion
- Data and Statistics
- Prevention Projects and Partners
Related Topics
Contact Info
Healthcare-Acquired Infections and Antibiotic Resistance in Minnesota Frequently Asked Questions
On this page:
What are health care-associated infections (HAIs)?
What is antibiotic resistance?
How are HAIs and antibiotic resistance connected?
How are HAIs and antibiotic resistance measured in Minnesota?
What are health care-associated infections (HAIs)?
HAIs are infections that people get while being treated in a health care facility, including hospitals, long-term care centers, outpatient clinics, dialysis centers, and surgery centers.
- HAIs are associated with a variety of causes including:
- Medical devices, such as catheters and ventilators
- Complications following a surgical procedure
- Complications of using antibiotics
- Some major HAIs in Minnesota include:
- Central line-associated bloodstream infections (CLABSI)
- Catheter-associated urinary tract infections (CAUTI)
- Surgical site infections (SSI)
- Clostridium difficile infections
- Methicillin-resistant Staphylococcus aureus (MRSA) bacteremia (i.e. bloodstream infection)
What is antibiotic resistance?
Antibiotics are powerful tools for fighting and preventing infections. Antibiotics kill bacteria and have made many medical advancements possible, such as surgery, cancer treatments, and intensive care medicine.
Antibiotic resistance occurs when bacteria change in a way that reduces or eliminates the effectiveness of antibiotics. This means the antibiotic is not able to kill the bacteria. Antibiotic-resistant infections have become more common and many bacteria have become resistant to more than one antibiotic. Any use of antibiotics can lead to more resistant bacteria in a person and in a community. Antibiotics need to be used wisely to keep new resistance from developing and prevent existing resistance from spreading. For example, antibiotics are used to treat infections caused by bacteria, not viruses. Treating a virus with an antibiotic does not treat the viral infection.
- Some major antibiotic-resistant infections in Minnesota include:
- Carbapenem-resistant-Enterobacteriaceae (CRE)
and Carbapenem-resistant-Acinetobacter - Invasive methicillin-resistant Staphylococcus aureus (MRSA)
- Streptococcus pneumoniae
- Group A and B Streptococcus (GAS, GBS)
- Extensively drug resistant tuberculosis (XDR-TB)
- Neisseria gonorrhoeae
- Campylobacter
- Non-typhoidal Salmonella
- Carbapenem-resistant-Enterobacteriaceae (CRE)
How are HAIs and antibiotic resistance connected?
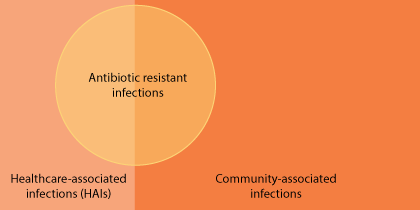
The issues of HAIs and antibiotic resistance overlap widely, but they are not the same. HAIs are often caused by antibiotic-resistant bacteria, but not always. Examples of HAIs caused by resistant bacteria include MRSA and CRE. Antibiotic-resistant bacteria are responsible for some HAIs but can also cause infections in the community such as resistant pneumococcal infections or community-associated MRSA. Antibiotic resistant infections can also occur in animals and resistant bacteria and their genes can be found in the environment.
- Common strategies can be used to address both HAIs and antibiotic resistance, including:
- Surveillance to measure the problem and the impact of prevention and control interventions
- Prevention of HAIs and slowing the emergence of antimicrobial resistance (e.g. infection control practices, vaccines to prevent infections, careful antibiotic prescribing)
- Research into better diagnostics, new vaccines and new antibiotics
How are HAIs and antibiotic resistance measured in Minnesota?
Minnesota has a variety of surveillance programs used to measure HAIs and antibiotic resistance in the state.
- Reportable Infectious Diseases
- Statewide
- Most recent changes to the communicable disease rule became effective in 2005
- Includes: Streptococcus pneumoniae, Group A and B Streptococcus (GAS, GAS), Extensively drug resistant tuberculosis (XDR-TB), Neisseria gonorrhoeae, Campylobacter, Non-typhoidal Salmonella infections, and pathogens causing Central line-associated bloodstream infections (CLABSI), Catheter-associated urinary tract infections (CAUTI), selected surgical site infections (SSI)
- Clostridium difficile Surveillance
(Clostridium difficile Reporting)- Five non-metro counties: Benton, Morrison, Olmstead, Stearns, and Todd Counties
- Started in 2009, Olmsted County added in 2012
- Includes: Clostridium difficile infections
- Multi-Site Gram-Negative Bacilli Surveillance
(CRE Surveillance Case Definition and Reporting)- Statewide
- Hennepin and Ramsey county started in 2011, statewide in 2016
- Includes: Carbapenem-resistant-Enterobacteriaceae, Carbapenem-resistant-Acinetobacter infections
- Active Bacterial Core (ABCs) Surveillance
(Invasive Bacterial Disease Surveillance, Invasive Staphylococcus aureus Surveillance)- Statewide except for MRSA surveillance which is conducted in Hennepin and Ramsey Counties
- Started in 1997 except for MRSA surveillance which started in 2005 (although Ramsey county was added in 2007)
- Includes: Streptococcus pneumoniae, Group A and B Streptococcus (GAS, GBS), Methicillin-resistant Staphylococcus aureus (MRSA) bacteremia (i.e. bloodstream infection) and Invasive MRSA infections
- Foodborne Diseases Active Surveillance Network (FoodNet)
(Foodborne Illness Active Disease Surveillance)- Statewide
- Started in 1996-1997
- Includes: Campylobacter, Non-typhoidal Salmonella infections
- CDC: State-based HAI prevention: Minnesota
- National Healthcare Safety Network (NHSN) data
- Hospitals reporting to NHSN statewide as driven by Centers for Medicare and Medicaid Services (CMS) requirements (e.g. 143 hospitals in 2014)
- State-specific HAI reports produced annually since 2009
- Includes: Central line-associated bloodstream infections (CLABSI), Catheter-associated urinary tract infections (CAUTI), selected surgical site infections (SSI), Clostridium difficile infections, Methicillin-resistant Staphylococcus aureus (MRSA) bacteremia (i.e. bloodstream infection) and Invasive MRSA infections
- CDC: Antibiotic Resistance & Patient Safety Portal
- National Healthcare Safety Network (NHSN) data
- Hospitals reporting to NHSN statewide as driven by Centers for Medicare and Medicaid Services (CMS) requirements
- Data from 2011-2014
- Includes: 31 antibiotic-resistant bacteria associated with Central line-associated bloodstream infections (CLABSI), Catheter-associated urinary tract infections (CAUTI), selected surgical site infections (SSI)
- CDC NARMS Now: Human Data
- Emerging Infections Program (EIP) surveillance data
- Statewide
- Data from 1999-2013
- Includes: Campylobacter, Non-typhoidal Salmonella
- CDC: Gonococcal Isolate Surveillance Project (GISP)
- Hennepin county public health clinic data
- Started in 1998
- Includes: Neisseria gonorrhoeae